Dr. Jeanette Moody was appointed as Quality Management Officer of VA Sierra Pacific Network, VISN 21 (Pleasant Hill, California) on July 11, 2022. Prior to this role, Dr. Moody held the role of Deputy Quality Management Officer of the VA Sierra Pacific Network, VISN 21.
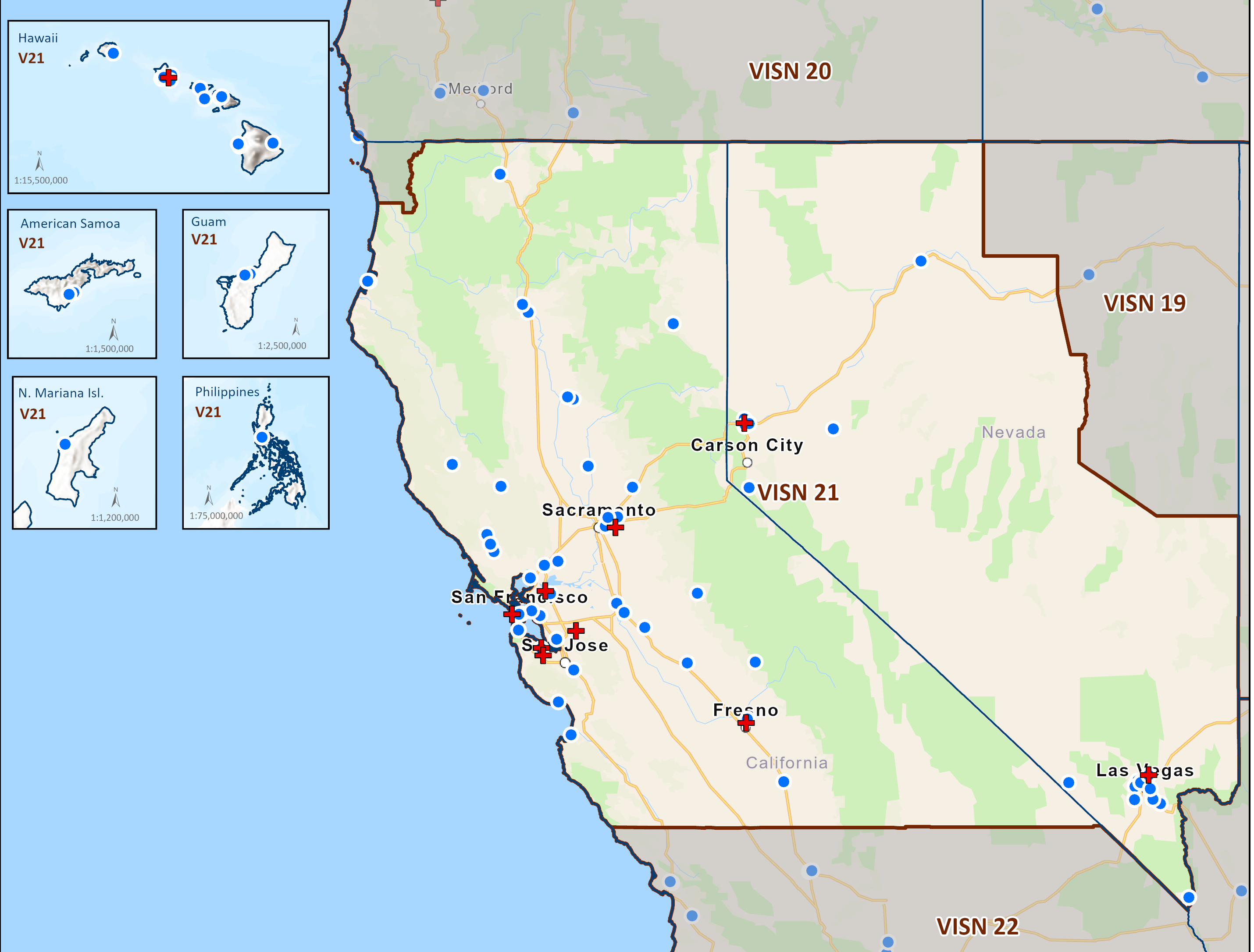
In her current role, Dr. Moody oversees the quality, safety, and high reliability in the Network with executive oversight of seven VA Health Care Systems in Northern and Central California, Nevada, Hawaii, Philippines and U.S. Territories in the Pacific Basin, 59 Community Based Outpatient Clinics. She holds direct full-line authority and responsibility for Patient Safety, Risk Management, Systems Redesign & Innovation, Performance Improvement, Accreditation & Regulatory Oversight and High Reliability for the region.
Dr. Moody holds a Doctor of Nursing Practice degree from Texas Tech University Health Sciences Center in Lubbock, Texas.; MSN degree from the University of Missouri-St. Louis in St. Louis, Missouri and a MBA degree from Texas Woman’s University in Houston, Texas. As a complement her nursing education and risk background, Dr. Moody holds a Doctor of Jurisprudence degree from Texas Tech School of Law. Dr. Moody is also a Certified Professional of Health Care Quality (CPHQ) and she is certified in Patient Safety (CPPS), Nursing Practice (CENP), and Advanced Nurse Executive competencies (NEA-BC).
Dr. Moody has served in various roles within the VA since 2013. Her previous roles included Director of Quality, Safety, and Value, Quality Manager, Accreditation Specialist, and Quality Consultant. Prior to joining the VA, Dr. Moody held several leadership and executive roles in the private health care sector throughout Missouri and Texas to include Service Line Manager, Branch Manager, Chief Quality Manager, Director of Nursing, Director of Clinical Operations, Director of Patient Care Services and Regional Director of Business and Clinical Operations.
Dr. Moody’s work has always been focused on advocating for Veteran care and the staff who serve while ensuring excellence and compliance with quality and regulatory standards.